"Breaking the silence, isolation and pain of eating disorders & bringing hope and support to those touched by them"
The Silver Linings Foundation
Eating disorders are real, complex and devastating conditions that can have serious consequences for health, productivity, and relationships. They are not a fad, phase or lifestyle choice and are often misunderstood. We discuss the general facts, causes, signs and statistics about eating disorders. Eating disorders have the highest mortality rate of any mental illness
Founded in the spring of 2014 by concerned parents and community members, Calgary Silver Linings Foundation builds awareness for eating disorders in Alberta and advances the development of urgently needed treatment programs and services.
In the summer of 2022, The Silver Linings Foundation, in collaboration with J5 Design, embarked on a journey to understand the current state of eating disorder experiences and identify new areas for growth. Designing with, not for was an integral part of our work; we strove to bring meaning and impact into the project by leveraging the power of storytelling. Our goal was to curate a safe space to invite clients to think with us, tell stories about their lived experiences, and gain a deeper understanding of the system.
In collaboration with Annand Olliviere & Rochelle Simons. Final Journey Map by Cindy Lam.
The Design Challenge
Understanding the current state of eating disorder experiences and identify new areas for growth and development that could better support youth and families to recover and begin to build the foundations for a healthy and thriving life.
26 INTERVIEWS / 4 WORKSHOPS / ∞ STORIES
We conducted 26 interviews with parents, healthcare professionals, and youth who have previously been or are currently struggling with an eating disorder. We heard stories about the challenges of navigating the system, the isolation and loneliness of the journey, the alienation they feel, the stigma that is associated with EDs, what atypical presentation is, and how we are currently not equipped or trained in recognizing EDs in Black, Indigenous, POC, or in refugees or those with intergenerational traumas. This was really the first phase of the project: to learn as much as we could.
1. Foundation for Dialogue
We initiated a series of workshops engaging families, youth, and healthcare professionals, setting the stage with discussions on collective futures and the envisioned world. These conversations served as the foundation for understanding the intricacies of the system.
2. Navigating the System
Recognizing the importance of comprehending the interconnectedness of system components, we adopted the human ecology model, revealing an existing network with communication gaps and silos. Our goal shifted to enhance communication within the system, directly impacting the patient experience
3. Stories as a Binding Force
Utilizing stories as a cohesive element, we conducted a journey mapping activity in workshops with families and youth. Overcoming the challenge of uniting diverse narratives, this activity proved impactful, fostering unity and validation among participants who often felt isolated due to the system's discouragement of communication.
.
4. Metaphors of Experience
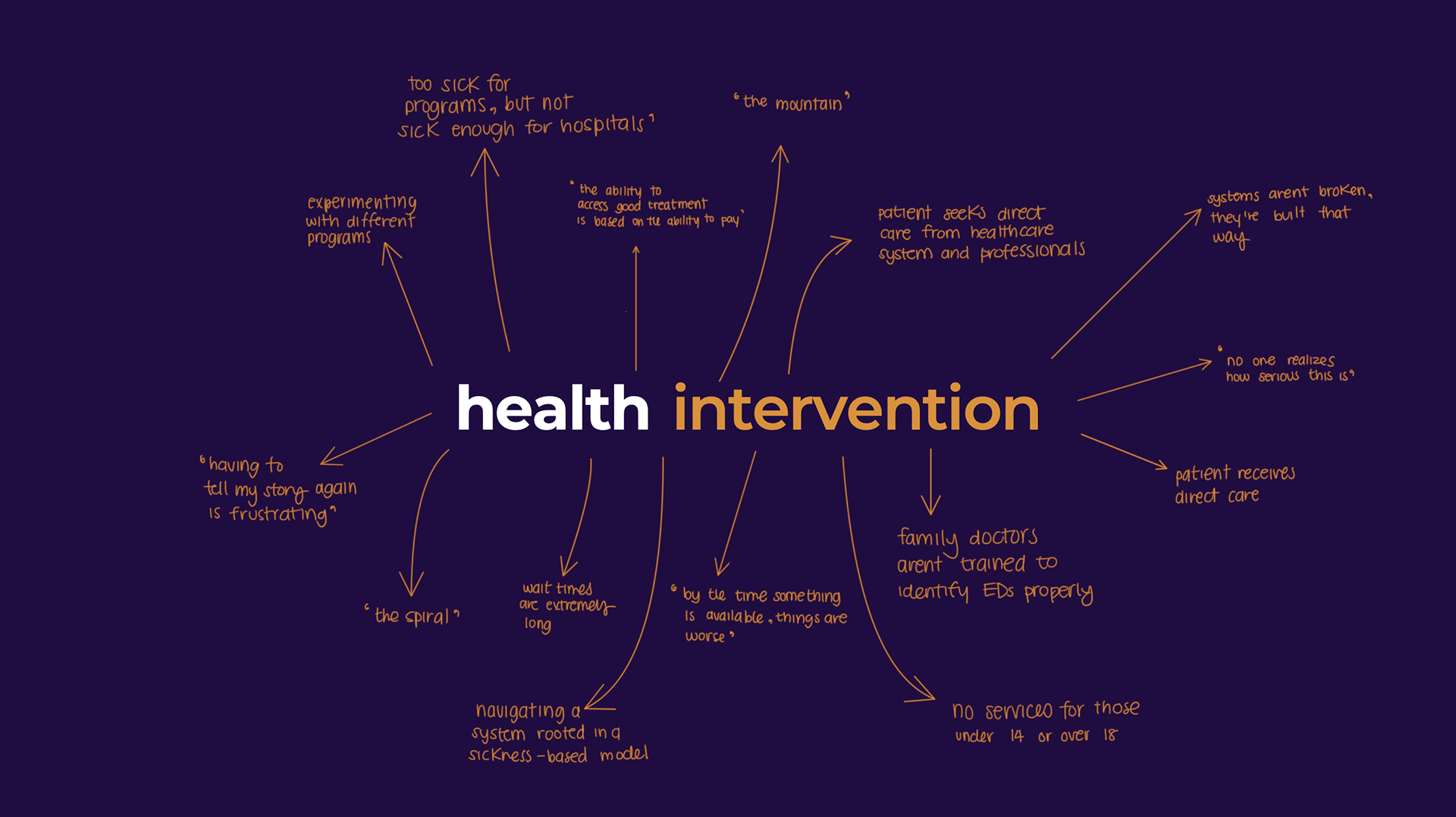
Participants vividly described phases of their journeys using metaphors. The period between diagnosis and treatment became the 'black hole,' treatment was labeled a 'spiral,' and transitions were referred to as 'walls' and 'mountains.' These metaphors provided a compelling and tangible way to convey challenges and emotions associated with each phase, offering unique insights.
Opportunity Statement
There is an opportunity to connect youth + families to early, reliable and integrated resources during their eating disorder journey in order to provide pathways of support rooted in a holistic care model.
Building community through coherence and empathy and weaving together the different threads to create a unifying narrative.
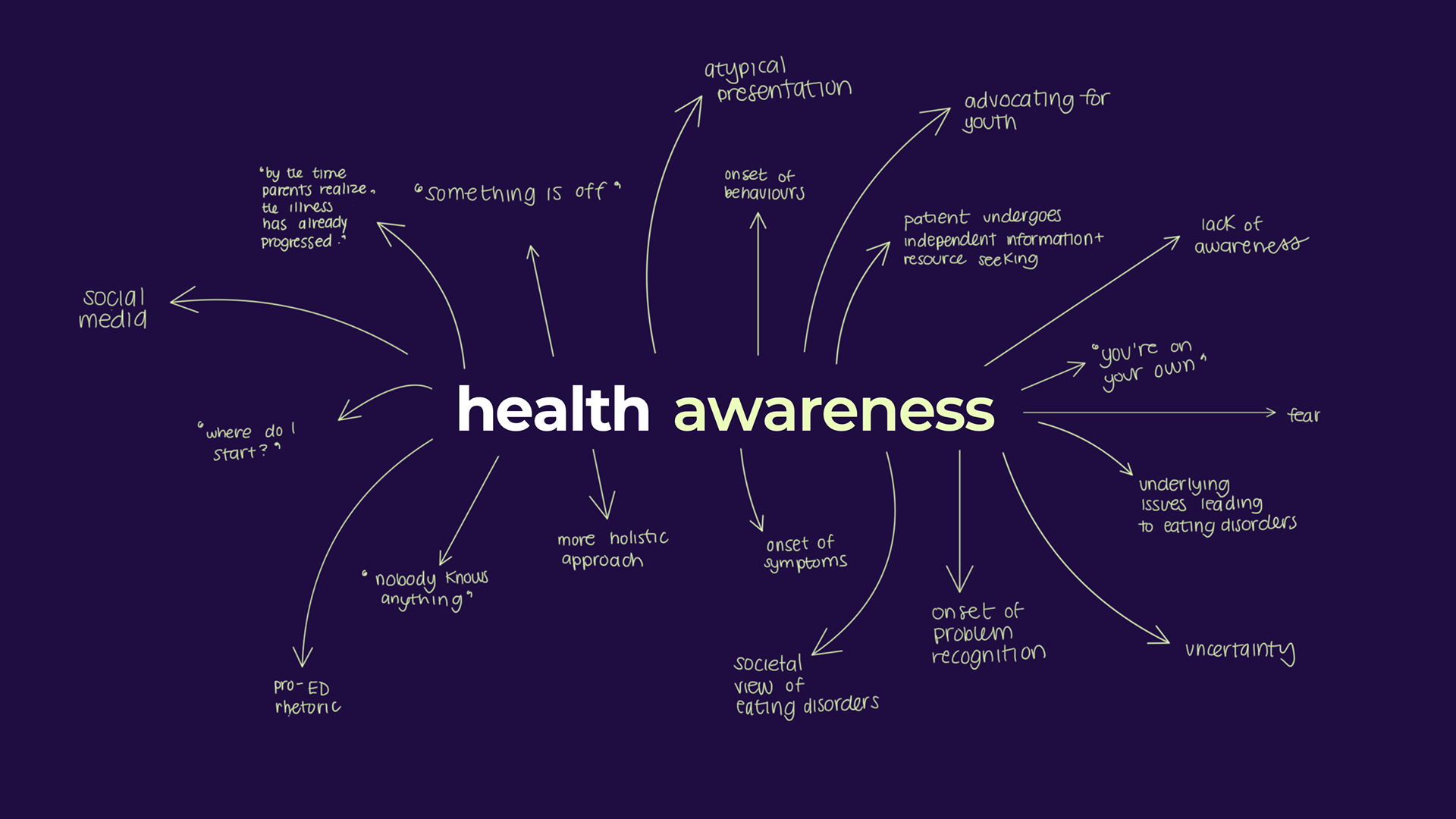
Synthesizing our findings from the initial workshops, we reorganized the journey into three distinct phases: health awareness, health intervention, and health management. This restructuring aimed to present a more holistic perspective, incorporating the varied experiences and insights we had gathered. Our deliberate use of the term "health" aimed to shift focus away from the system's tendency to emphasize visible aspects of eating disorders. Unlike conventional metrics, such as the cessation of purging for individuals with bulimia, our approach acknowledged that recovery manifests in diverse ways. Success could involve moments of reflection, even if followed by a return to previous patterns. Unfortunately, these nuanced successes often escape recognition within the existing framework. The choice of "health" sought to foster a broader understanding, encouraging a more comprehensive outlook beyond traditional metrics.
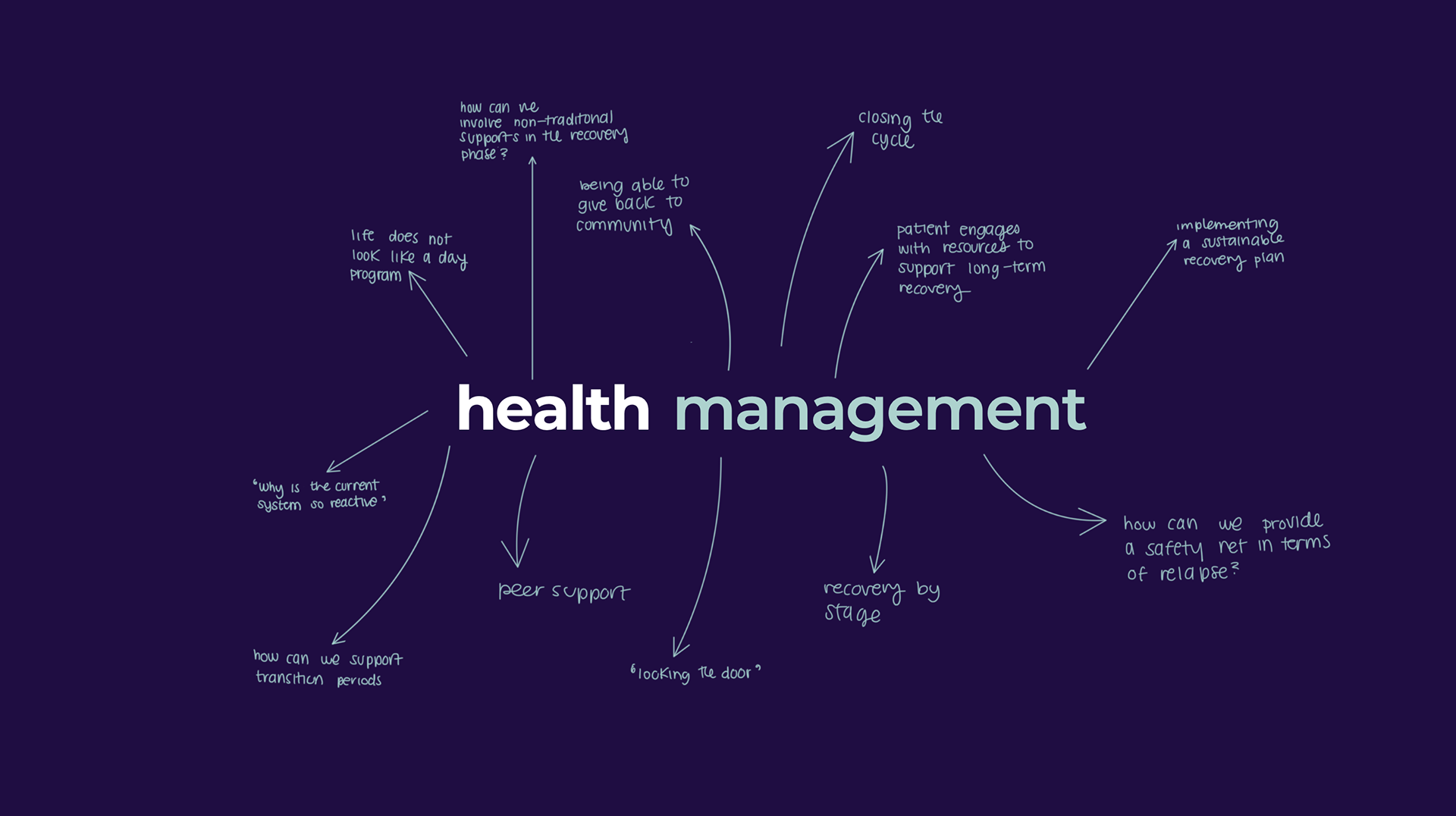
We presented the opportunity statement to healthcare professionals, aligning with the insights gathered from the youth sessions. An ongoing challenge was bridging insights from these separate sessions, prompting the decision to facilitate family and youth, as well as healthcare professionals, in distinct workshops to maintain a secure environment. During the final workshops, sharing the opportunity statement marked a breakthrough. Professionals and families & youth exhibited alignment, in stark contrast to the initial series where differences were pronounced. To address this intricate problem comprehensively, we initiated low-fidelity prototyping. Employing how-might-we (HMW) questions aligned with opportunities and challenges identified in previous sessions, we tied each HMW to different phases of the patient journey. Clients and professionals ideated, voted on the strongest concepts, and storyboarded potential ideas to address barriers or enhance aspects of the journey. This phase, requiring a transition from ideation to tangible creation, posed a unique challenge for participants.
This in practice is embodying the principle of designing with, not for —catering these prototypes directly for the youth and families who are the ones most impacted in this journey.
Solution: Mobile Training
In collaboration with the Eating Disorder Support Network of Alberta (EDSNA), The Silver Linings Foundation will launch a program named “Train the Trainer,” responding to an opportunity area identified by healthcare professionals in the prototyping workshops. Aligned with the HMW question "How might we shift the approach to recognizing disordered eating beyond the current reliance on a sickness-based medical model?" this mobile program involves trained individuals offering learning and capacity building services to touch-points and organizations engaging youth. Trainers could disseminate relevant information and training to schools, non-profit organizations, sports and recreation clubs, places of worship, primary and public health centers, and parenting groups. The training encompasses educating on best practices for discussing wellbeing, consulting with educators to adjust curriculums, assisting coaches in supporting athletes, and building skills for parents to guide children through puberty. This approach aims to shift mindsets and enhance skill sets, ultimately reducing the root factors contributing to disordered eating over time.

